Bone infections are prevalent disease and found worldwide but the pattern of the disease is getting altered. Now-a-days the bone infections are more often following complex trauma, surgical procedures, and peripheral vascular disease and also as sequel of diabetes. The use of antibiotics had improved the outcome in severe diseases but that accounts only few cases and majority are those that requires surgery in addition to antibiotics.
Acute osteomyelitis usually can cause severe systemic upset and even mortality whereas the chronic osteomyelitis presents with chronic pain, discharging sinus, associated unemployment, social burden, repeated medical care need and can associate with high risk of mental illnesses like depression.
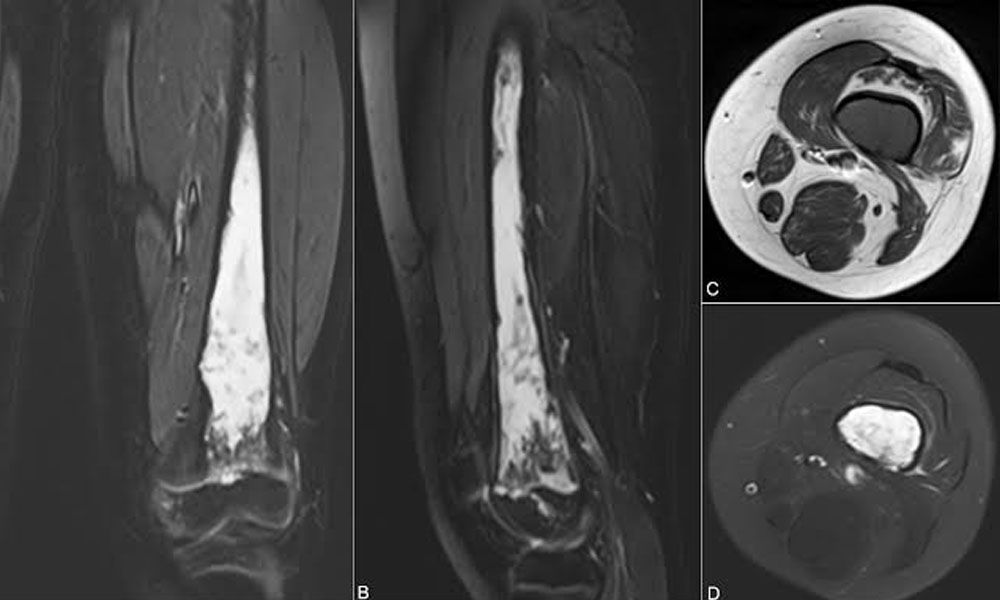
Hence treatment of chronic osteomyelitis needs to be aggressive to eliminate the infective foci to prevent its recurrence. In approach to achieve it might require radical removal of infected bone and adjacent soft tissues resulting with wide defect that usually needs reconstructive measures like free flaps to bridge it.
The treatment of chronic osteomyelitis is always been daunting and being infamous because of persisting infection and relapse.
The probable reasons can be various like inadequate debridement of infective foci (sequestrum and adjacent involved soft tissues), reduced blood flow to the area due to primary result or secondarily subsequent to operative procedures that causes decreased healing potential and diminished resistance to recurrent infection, severe scarring and dead space also acts as contributing factors for nidus of infection and chronicity of the disease and low oxygen tension leads to mixed microbial pattern(aerobic and anaerobic) and also forms biofilm that decreases the role of antibiotics to act at the foci of infection due to poor penetration to the site. The disease can present with discharging sinus, dull aching pain, pathological fracture, non-union and in severe form malignancy. From the various management modalities mentioned for chronic osteomyelitis in literature various methods includes antibiotic therapy, surgical debridement, skin grafting, local flaps, muscle flaps, distant cross leg flaps, bone grafting and bone transport. Although many among theses having its own limitations, as previously mentioned antibiotics having limitations because of poor penetration to foci of infection and due to resistant bacteria. Skin grafting and local flaps can have limitations because of limited debridement being done to avoid ending in a wide defect that becomes a challenge for reconstruction. Although pedicled muscle flaps are good options wherever applicable but it has anatomic limitations as in leg can be mostly used for proximal leg defects, but has got advantage over the local fascio-cutaneous flap as these flaps have low oxygen tension at its distal portion and those being critical area to be covered. Hence it’s been important to radically remove all the infective foci in soft tissue and bone with free flaps being in armamentarium to cover the soft tissue as well as the bony defect and subsequently giving antibiotics that increases the delivery of it due to increased blood supply from the transferred flap and hence reducing the probability of relapse of the disease.
So the treatment philosophy becomes similar to that in management of malignant tumour where we need to excise the tumour along with adjacent normal tissue to avoid any future relapse.
In view of this, similar to staging the malignancy consider to follow the Cierny-Mader classification for chronic osteomyelitis to organise the treatment plans considering the host’s immune status and physiological ability to effect healing.